상세 컨텐츠
본문
Bipolar and Related Disorders
Bipolar I Disorder
For a diagnosis of bipolar I disorder, it is necessary to meet the following criteria for a manic episode. The manic episode may have been preceded by and may be followed by hypomanic or major depressive episodes.
Manic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary).
B. During the period of mood disturbance and increased energy or activity, three (or more) of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior:
1. Inflated self-esteem or grandiosity.
2. Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
3. More talkative than usual or pressure to keep talking.
4. Flight of ideas or subjective experience that thoughts are racing.
5. Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
6. Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation (i.e., purposeless non-goal-directed activity).
7. Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others, or there are psychotic features.
D. The episode is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, other treatment) or to another medical condition.
Note: A full manic episode that emerges during antidepressant treatment (e.g., medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a manic episode and, therefore, a bipolar I diagnosis.
Note: Criteria A-D constitute a manic episode. At least one lifetime manic episode is required for the diagnosis of bipolar I disorder.
Hypomanic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 4 consecutive days and present most of the day, nearly every day.
B. During the period of mood disturbance and increased energy and activity, three (or more) of the following symptoms (four if the mood is only irritable) have persisted, represent a noticeable change from usual behavior, and have been present to a significant degree:
1. Inflated self-esteem or grandiosity.
2. Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
3. More talkative than usual or pressure to keep talking.
4. Flight of ideas or subjective experience that thoughts are racing.
5. Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
6. Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation.
7. Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The episode is associated with an unequivocal change in functioning that is uncharacteristic of the individual when not symptomatic.
D. The disturbance in mood and the change in functioning are observable by others.
E. The episode is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization. If there are psychotic features, the episode is, by definition, manic.
F. The episode is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, other treatment).
Note: A full hypomanic episode that emerges during antidepressant treatment (e.g., medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a hypomanic episode diagnosis. However, caution is indicated so that one or two symptoms (particularly increased irritability, edginess, or agitation following antidepressant use) are not taken as sufficient for diagnosis of a hypomanic episode, nor necessarily indicative of a bipolar diathesis.
Note: Criteria A-F constitute a hypomanic episode. Hypomanic episodes are common in bipolar I disorder but are not required for the diagnosis of bipolar I disorder.
Major Depressive Episode
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
Note: Do not include symptoms that are clearly attributable to another medical condition.
1. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, or hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.)
2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or de crease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.)
4. Insomnia or hypersomnia nearly every day.
5. Psychomotor agitation or retardation nearly every day (observable by others; not merely subjective feelings of restlessness or being slowed down).
6. Fatigue or loss of energy nearly every day.
7. Feelings of worthlessness or excessive or inappropriate quilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
9. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
C. The episode is not attributable to the physiological effects of a substance or another medical condition.
Note: Criteria A-C constitute a major depressive episode. Major depressive episodes are common in bipolar I disorder but are not required for the diagnosis of bipolar I disorder.
Note: Responses to a significant loss (e.g., bereavement, financial ruin, sses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode. Although such symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal re-Bipolar I Disorder sponse to a significant loss should also be carefully considered. This decision inevitably requires the exercise of clinical judgment based on the individual's history and the cultural norms for the expression of distress in the context of loss.¹
Bipolar I Disorder
A. Criteria have been met for at least one manic episode (Criteria A-D under "Manic Episode" above).
B. The occurrence of the manic and major depressive episode(s) is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorder.
¹In distinguishing grief from a major depressive episode (MDE), it is useful to consider that in grief the predominant affect is feelings of emptiness and loss, while in an MDE, it is persistent depressed mood and the inability to anticipate happiness or pleasure. The dysphoria in grief is likely to decrease in intensity over days to weeks and occurs in waves, the so-called pangs of grief. These waves tend to be associated with thoughts or reminders of the deceased. The depressed mood of an MDE is more persistent and not tied to specific thoughts or preoccupations. The pain of grief may be accompanied by positive emotions and humor that are uncharacteristic of the pervasive unhappiness and misery characteristic of an MDE. The thought content associated with grief generally features a preoccupation with thoughts and memories of the deceased, rather than the self-critical or pessimistic ruminations seen in an MDE. In grief, self- esteem is generally preserved, whereas in an MDE, feelings of worthlessness and self-loathing are common. If self-derogatory ideation is present in grief, it typically involves perceived failings vis-à-vis the deceased (e.g., not visiting frequently enough, not telling the deceased how much he or she was loved). If a bereaved individual thinks about death and dying, such thoughts are generally focused on the deceased and possibly about "joining" the deceased, whereas in an MDE, such thoughts are focused on ending one's own life because of feeling worthless, undeserving of life, or unable to cope with the pain of depression.
Coding and Recording Procedures
The diagnostic code for bipolar I disorder is based on type of current or most recent episode and its status with respect to current severity, presence of psychotic features, and remission status. Current severity and psychotic features are only indicated if full criteria are currently met for a manic or major depressive episode. Remission specifiers are only indicated if the full criteria are not currently met for a manic, hypomanic, or major depressive episode. Codes are as follows:
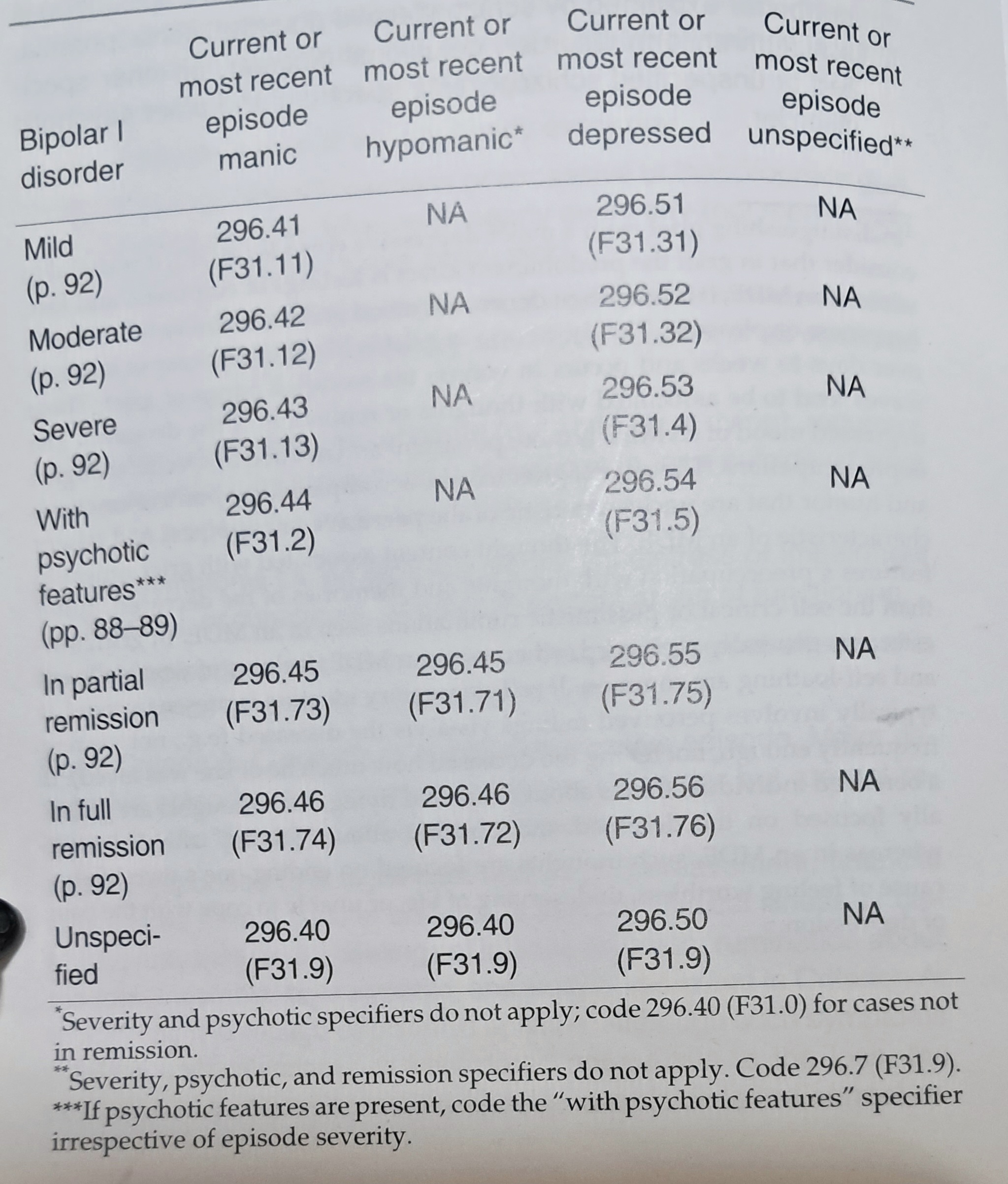
In recording the name of a diagnosis, terms should be listed in the following order: bipolar I disorder, type of current or most recent episode, severity/psychotic/remission specifiers, followed by as many specifiers without codes as apply to the current or most recent episode.
Specify:
With anxious distress (pp. 83-84)
With mixed features (pp. 84-86)
With rapid cycling (p. 86)
With melancholic features (pp. 86-87)
With atypical features (pp. 87-88)
With mood-congruent psychotic features (pp. 88-89)
With mood-incongruent psychotic features (pp. 88-89)
With catatonia (p. 89). Coding note: Use additional code 293.89 (F06.1).
With peripartum onset (pp. 89-90)
With seasonal pattern (pp. 90-92)
Bipolar II Disorder
296.89 (F31.81)
For a diagnosis of bipolar II disorder, it is necessary to meet the following criteria for a current or past hypomanic episode and the following criteria for a current or past major depressive episode:
Hypomanic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 4 consecutive days and present most of the day, nearly every day.
B. During the period of mood disturbance and increased energy and activity, three (or more) of the following symptoms have persisted (four if the mood is only irritable), represent a noticeable change from usual behavior, and have been present to a significant degree:
1. Inflated self-esteem or grandiosity.
2. Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
3. More talkative than usual or pressure to keep talking.
4. Flight of ideas or subjective experience that thoughts are racing.
5. Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
6. Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation.
7. Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The episode is associated with an unequivocal change in functioning that is uncharacteristic of the individual when not sympomatic.
D. The disturbance in mood and the change in functioning are observable by others.
E. The episode is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization. If there are psychotic features, the episode is, by definition, manic.
F. The episode is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication or other treatment).
Note: A full hypomanic episode that emerges during antidepressant treatment (e.g., medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a hypomanic episode diagnosis.
However, caution is indicated so that one or two symptoms (particularly increased irritability, edginess, or agitation following antidepressant use) are not taken as sufficient for diagnosis of a hypomanic episode, nor necessarily indicative of a bipolar diathesis.
Major Depressive Episode
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
Note: Do not include symptoms that are clearly attributable to a medical condition.
1. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, or hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.)
2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.)
4. Insomnia or hypersomnia nearly every day.
5. Psychomotor agitation or retardation nearly every day (observable by others; not merely subjective feelings of restlessness or being slowed down).
6. Fatigue or loss of energy nearly every day.
7. Feelings of worthlessness or excessive or inappropriate guilt(which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
9. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, a suicide attempt, or a specific plan for committing suicide.
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
C. The episode is not attributable to the physiological effects of a substance or another medical condition.
Note: Criteria A-C above constitute a major depressive episode.
Note: Responses to a significant loss (e.g., bereavement, financial ruin, losses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about ability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode. Although such symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should be carefully considered. This decision inevitably requires the exercise of clinical judgment based on the individual's history and the cultural norms for the expression of distress in the context of loss.2
Schizophrenia Spectrum and Other Psychotic Disorders - Delusional Disorder, Schizotypal (Personality) Disorder, Brief Psychotic
Schizophrenia Spectrum and Other Psychotic Disorders Schizotypal (Personality) Disorder Criteria for schizotypal personality disorder can be found in the chapter "Personality Disorders." Because this disorder is considered part of the schizophrenia spectru
psychologymind.tistory.com
Bipolar II Disorder
A. Criteria have been met for at least one hypomanic episode (Criteria A-F under "Hypomanic Episode" above) and at least one major depressive episode (Criteria A-C under "Major Depressive Episode" above).
B. There has never been a manic episode.
C. The occurrence of the hypomanic episode(s) and major depressive episode(s) is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorder.
²In distinguishing grief from a major depressive episode (MDE), it is useful to consider that in grief the predominant affect is feelings of emptiness and loss, while in an MDE, it is persistent depressed mood and the inability to anticipate happiness or pleasure. The dysphoria in grief is likely to decrease in intensity over days to weeks and occurs in waves, the so-called pangs of grief. These waves tend to be associated with thoughts or reminders of the deceased. The depressed mood of an MDE is more persistent and not tied to specific thoughts or preoccupations. The pain of grief may be accompanied by positive emotions and humor that are uncharacteristic of the pervasive unhappiness and misery characteristic of an MDE. The thought content associated with grief generally features a preoccupation with thoughts and memories of the deceased, rather than the self-critical or pessimistic ruminations seen in an MDE. In grief, self-esteem is generally preserved, whereas in an MDE, feelings of worthlessness and self loathing are common. If self-derogatory ideation is present in grief, it typically involves perceived failings vis-à-vis the deceased (e.g., not visiting frequently enough, not telling the deceased how much he or she was loved). If a bereaved individual thinks about death and dying, such thoughts are generally focused on the deceased and possibly about "joining" the deceased, whereas in an MDE, such thoughts are focused on ending one's own life because of feeling worthless, undeserving of life, or unable to cope with the pain of depression.
D. The symptoms of depression or the unpredictability caused by frequent alternation between periods of depression and hypomania causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Coding and Recording Procedures
Bipolar II disorder has one diagnostic code: 296.89 (F31.81). Its status with respect to current severity, presence of psychotic features, course, and other specifiers cannot be coded but should be indicated in writing (e.g., 296.89 [F31.81] bipolar II disorder, current episode depressed, moderate severity, with mixed features; 296.89 [F31.81] bipolar Il disorder, most recent episode depressed, in partial remission).
Specify current or most recent episode:
Hypomanic
Depressed
Specify if:
With anxious distress (pp. 83-84)
With mixed features (pp. 84-86)
With rapid cycling (p. 86)
With mood-congruent psychotic features (pp. 88-89)
With mood-incongruent psychotic features (pp. 88-89)
With catatonia (p. 89). Coding note: Use additional code 293.89 (F06.1).
With peripartum onset (pp. 89-90)
With seasonal pattern (pp. 90-92): Applies only to the pattern of major depressive episodes.
Specify course if full criteria for a mood episode are not currently met:
In partial remission (p. 92)
In full remission (p. 92)
Specify severity if full criteria for a mood episode are currently met:
Mild (p. 92)
Moderate (p. 92)
Severe (p. 92)
DESK REFERENCE TO THE DIAGNOSTIC CRITERIA FROM DSM-5
2023.10.14 - [임상심리학/DSM-5] - Schizophrenia/Schizoaffective Disorder
Schizophrenia/Schizoaffective Disorder
Schizophrenia 295.90 (F20.9) Schizophrenia A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of these must be (1), (2), or (3): 1. Delusions. 2. Halluci
psychologymind.tistory.com
'임상심리학 > DSM-5' 카테고리의 다른 글
| Psychotic Disorder Due to Another Medical Condition/Cataonia - Catatonia Associa (0) | 2023.10.19 |
|---|---|
| Substance/Medication-Induced Psychotic Disorder (0) | 2023.10.19 |
| Schizophrenia Spectrum and Other Psychotic Disorders - Delusional Disorder, Schi (0) | 2023.10.14 |
| Schizophrenia/Schizoaffective Disorder (0) | 2023.10.14 |
| 피학성 성격장애(Criteria for Masochistic Personality Disorder)의 진단기준 (0) | 2023.06.29 |




